How the Gut–Brain Axis and Headaches Are Connected: An Osteopathic Perspective
November 19, 2025
Supplements + Concussion Recovery
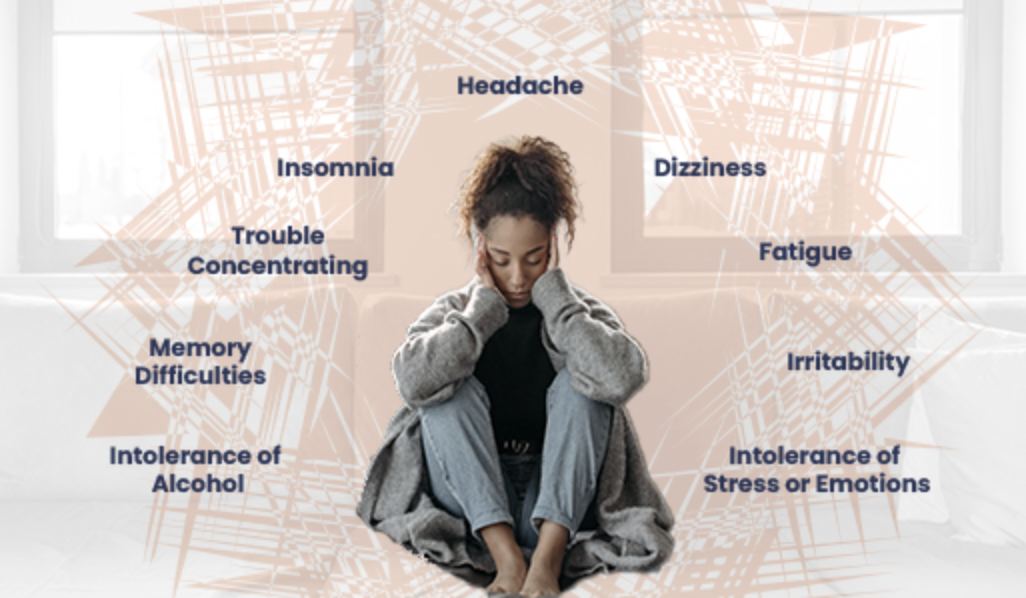
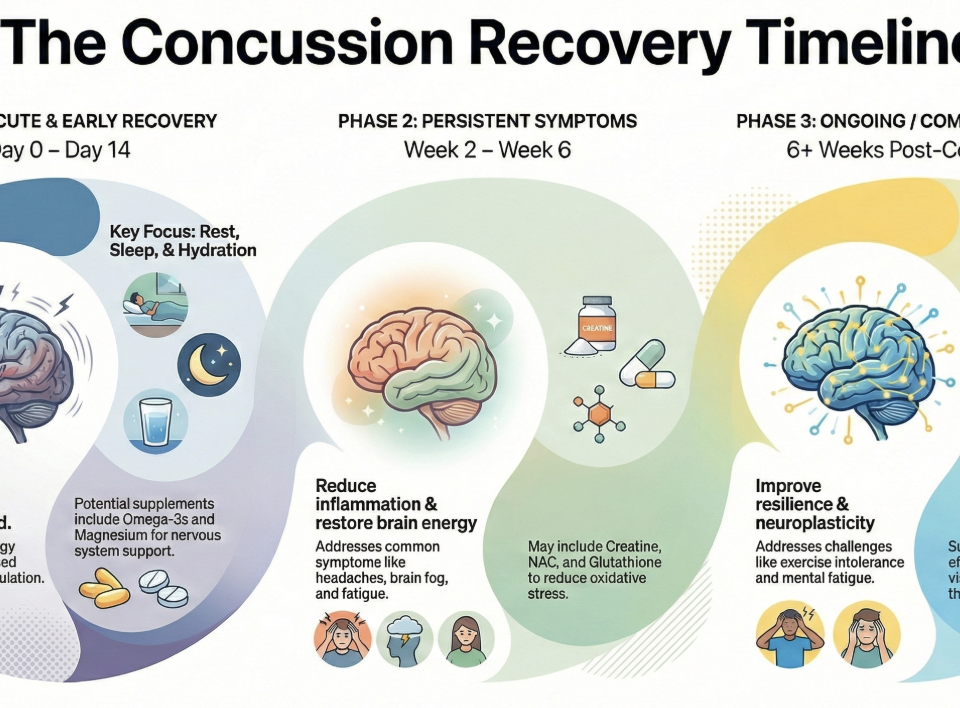
February 2, 2026If you are still experiencing headaches, brain fog, fatigue, or exercise intolerance months after a concussion, you may have been told your MRI is normal and that your brain has “healed.” For many people with Persistent Post-Concussion Symptoms (PPCS), this disconnect is frustrating and confusing.
The reality is that PPCS is rarely caused by ongoing structural brain damage such as a bruise or bleed. Instead, symptoms persist because of functional dysregulation, particularly involving neuroinflammation and the autonomic nervous system (ANS).
Understanding PPCS requires a systems-based approach, recognising how the brain, immune system, and nervous system interact. Below, we explore why recovery gets “stuck” and how osteopathic management can help reset the system.
The Feed-Forward Loop: Why Symptoms Persist After Concussion
In a typical concussion recovery, the body activates protective responses and then gradually returns to baseline. In PPCS, these responses fail to fully switch off.
The immune system and autonomic nervous system enter a feed-forward loop, where dysfunction in one system amplifies the other. Autonomic overactivation keeps the body in a state of threat, while persistent immune signalling maintains metabolic stress within the brain.
The result is a reduced energy ceiling, where even small physical, cognitive, or emotional loads trigger symptom flare-ups.
Neuroinflammation: When Repair Becomes Maladaptive
Neuroinflammation is a normal part of early concussion recovery. However, when it becomes chronic, it shifts from healing to symptom generation.
How neuroinflammation contributes to PPCS
Mechanism
Advanced imaging and biomarker research show that microglial activation, the brain’s immune response, can persist for months following concussion.
Clinical effects
- Cognitive fatigue and brain fog
Ongoing inflammation increases metabolic demand and reduces neural efficiency, leading to slowed thinking and mental exhaustion. - Headache and sensory sensitivity
Inflammatory signalling sensitises pain pathways, particularly trigeminal networks, lowering headache thresholds. - Mood and sleep disruption
Inflammatory mediators interfere with neurotransmitter balance, affecting emotional regulation and sleep quality.
Autonomic Dysregulation: The Nervous System Stuck in High Gear
The autonomic nervous system controls heart rate, blood pressure, breathing, digestion, and stress responses. In PPCS, this system often loses adaptability.
What autonomic dysfunction looks like after concussion
Mechanism
Patients frequently demonstrate reduced heart rate variability (HRV) and impaired cardiovascular responses to stress, reflecting a loss of physiological flexibility.
Common symptoms
- Exercise intolerance
Difficulty regulating cerebral blood flow during exertion causes symptom flares with physical activity. - “Wired but tired”
Persistent sympathetic dominance leads to hyperarousal, poor sleep, and non-restorative fatigue. - Dizziness and palpitations
Orthostatic symptoms may resemble conditions such as POTS (Postural Orthostatic Tachycardia Syndrome).
How Osteopathic Treatment Helps Break the PPCS Cycle
Effective PPCS care shifts focus from “brain damage” to nervous system regulation. Osteopathic management supports recovery by reducing physical drivers of threat and restoring autonomic balance.
1. Optimising breathing and autonomic regulation
Breathing directly influences the autonomic nervous system. Rib cage, thoracic spine, and diaphragm restrictions often lead to shallow, chest-based breathing, reinforcing sympathetic dominance.
Osteopathic approach
Manual treatment to the ribs and thoracic spine improves respiratory mechanics, supports vagal tone, and helps shift the body out of chronic “fight-or-flight.”
2. Reducing ongoing pain and threat signals
Pain itself is a stressor. Dysfunction in the cervical spine, upper thoracic region, and TMJ continuously feeds nociceptive input into the nervous system.
Osteopathic approach
By addressing neck and jaw dysfunction, osteopathic care reduces peripheral threat signals, helping dampen sympathetic overactivation and headache sensitivity.
3. Expanding tolerance to activity and rehabilitation
Autonomic dysfunction limits exercise tolerance, making rehabilitation feel impossible.
Osteopathic role
Improved biomechanics and reduced baseline load increase a patient’s energy envelope, allowing safe progression into graded aerobic and strength-based rehabilitation a key driver of long-term autonomic normalisation.
Conclusion: Why a Systems Approach Matters in PPCS
Persistent post-concussion symptoms are real, physical, and reversible. They are driven not by ongoing brain damage, but by a failure of the body’s regulatory systems to return to balance.
By addressing neuroinflammation, autonomic dysregulation, and ongoing physical stressors through osteopathic management and structured rehabilitation, recovery can restart and momentum can be restored.